Beginning in October 2023, providers who participate in our PCP Quality Incentive Program (PQIP) began seeing additional health equity data reflected in their Gaps in Care reporting. This new data indicates how members of your panel of different races and ethnicities are performing relative to various HEDIS® measures. We’re now providing it to help you ensure your patients are receiving equitable care.
You will now see additional data points for Medicare Advantage members in your panel related to their disability and income status. We’re providing this information to you so we can work together to improve the health and wellness of your patients, our members, and all Rhode Islanders.
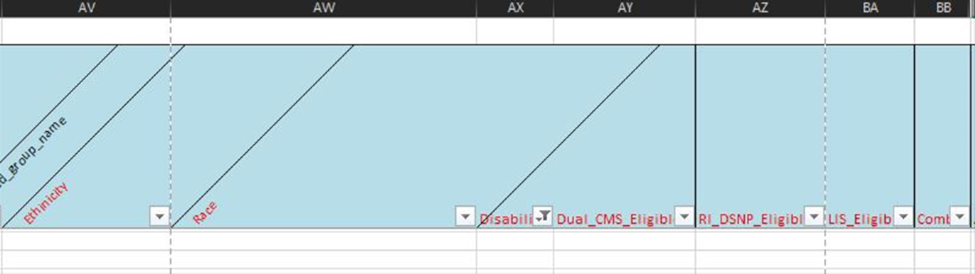
Below is an example of how the new Health Equity Indicators will appear on the member-level detail reports. In columns AV - BB you will see the following indicators (reference key below):
- Race: The race assigned to a member
- Ethnicity: The ethnicity assigned to a member
- Disability: Member is identified to have a disability
- Dual_CMS_Eligible: Members eligible to be in duals CMS population
- RI_DSNP_Eligible: Subset of duals CMS population; in Rhode Island D-SNP population
- LIS_Eligible: Members who are eligible low-income status
- Combo: Members who are eligible for LIS_Eligible and disability
If you have any questions about your reporting, please contact the Quality Concierge Team at QualityHEDIS@bcbsri.org.