Improving post-fracture care for at-risk patients
As a healthcare provider, actively addressing osteoporosis management following a fracture is essential to improving patient outcomes and reducing the risk of future fractures. This article outlines post-fracture osteoporosis care, review period details, and actionable steps for engaging patients in effective prevention and treatment strategies.
Measure defined
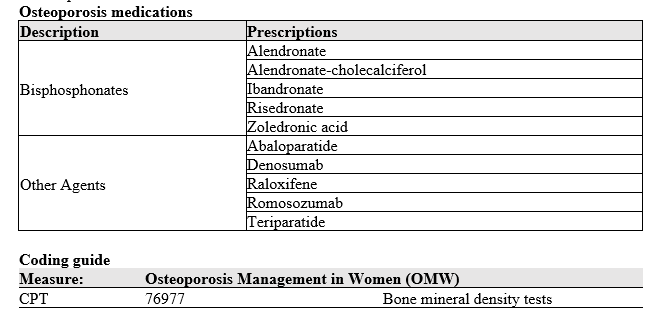
The percentage of the population who had either a bone mineral density (BMD) test or prescription for a drug to treat osteoporosis in 180 days (six months) after the fracture. Fractures of finger, toe, face, and skull are not included in the measure.
Review period
7/1/2025 – 06/30/2026
Refer to the monthly report distributed by the BCBSRI Quality team, which identifies patients within your practice who have recently experienced a fracture and require a bone mineral density assessment.
Best practices and patient communication tips
- Encourage patients to maintain healthy lifestyle choices, including a proper diet, weight-bearing exercises, and adherence to prescribed medication to prevent further bone loss.
- Discuss an individualized fall prevention plan with each patient, such as removing home hazards (e.g., area rugs), using night lights, and installing grab bars or handrails.
- Assist patients in scheduling a BMD assessment and provide a prescription for osteoporosis treatment when clinically indicated.
- By consistently implementing these best practices, providers play a critical role in reducing osteoporosis-related complications and supporting the long-term health of their patients.
If you have any questions on the PQIP Program, quality management, or would like further details, please contact the BCBSRI Quality Team at QualityHEDIS@bcbsri.org. The team is always available to answer questions.

